When we think of therapy, we usually picture talking to a counselor or taking medication.
But what if the brain could be trained to improve its own patterns? That’s the idea behind Neurofeedback Therapy, also called EEG biofeedback—a non-invasive method that uses real-time brainwave feedback to guide healthier activity.
The Neurofeedback market is currently valued at $1.4 billion and is projected to grow to $2.03 billion by 2030. All this investment shows the rapid progress and interest in clinical trials and the practice of Neurofeedback.
In this guide, we’ll explore what it is, how it works, its types, benefits, and what to expect in a session.
What Is Neurofeedback Therapy?
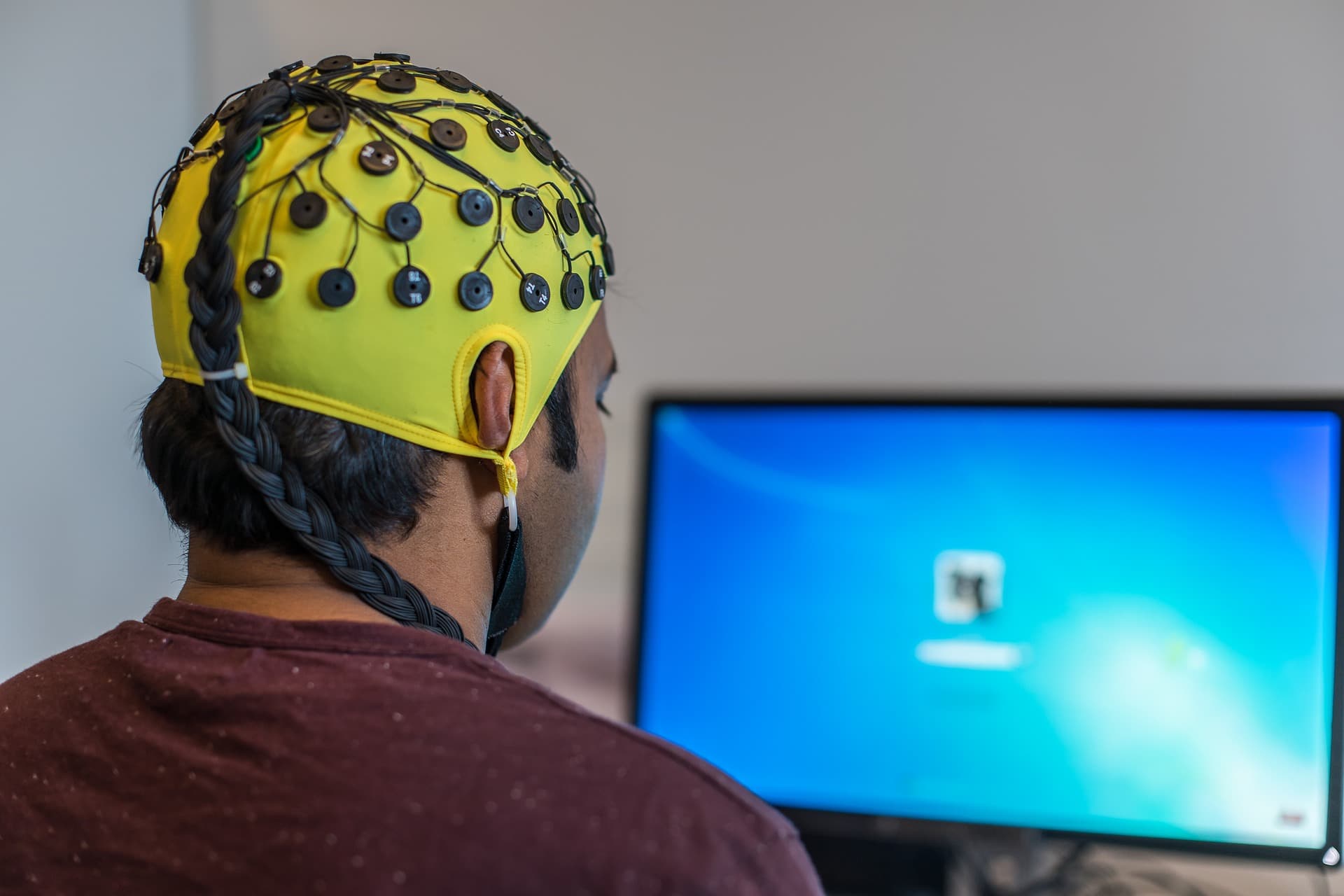
Neurofeedback therapy is a training method where sensors (often EEG) monitor your brain’s electrical activity. You get feedback (usually sounds or visuals) about what your brain is doing in real-time.
Then, using that feedback, your brain can learn to shift its activity toward more helpful patterns (for example, calmer waves or more focused waves).
It differs from traditional talk therapy (discussing thoughts and behavior) and drug therapy (which changes brain chemistry) because here you are guiding the brain’s own activity.
In comparison to traditional CBT therapy, in a study in Iran, Neurofeedback has shown better short-term results and comparable long-term results to CBT.
The main idea is brainwave training, which is strengthening or reducing specific frequencies of brain waves in certain places, so mental states such as attention, calmness, and sleep improvement.
History & Development Of Neurofeedback
Neurofeedback has a rich history of scientific breakthroughs that have moved it from pure theory to a proven clinical tool.
The concept of brainwave training was pioneered in the 1960s by scientists like Dr. Joe Kamiya. He showed that people could voluntarily learn to control their own alpha brain waves, a key step in showing that the brain could be trained.
A second major breakthrough came from Dr. Barry Sterman’s work with cats, where he trained cats to produce a specific brainwave pattern called the sensorimotor rhythm (SMR).
When these same cats were later exposed to a toxic rocket fuel that caused seizures in all the untrained cats, the neurofeedback-trained cats were surprisingly resistant.
Sterman’s discovery provided the first solid evidence that brainwave training could have tangible, physiological effects.
The field was further revolutionized in the 1980s by the advancements of Quantitative Electroencephalography (qEEG).
This technology allowed clinicians to create a “brain map” by comparing a patient’s brainwave patterns to a large database of healthy brains. This innovation changed neurofeedback from a generalized training method into a targeted, evidence-based therapy.
How Does Neurofeedback Work?
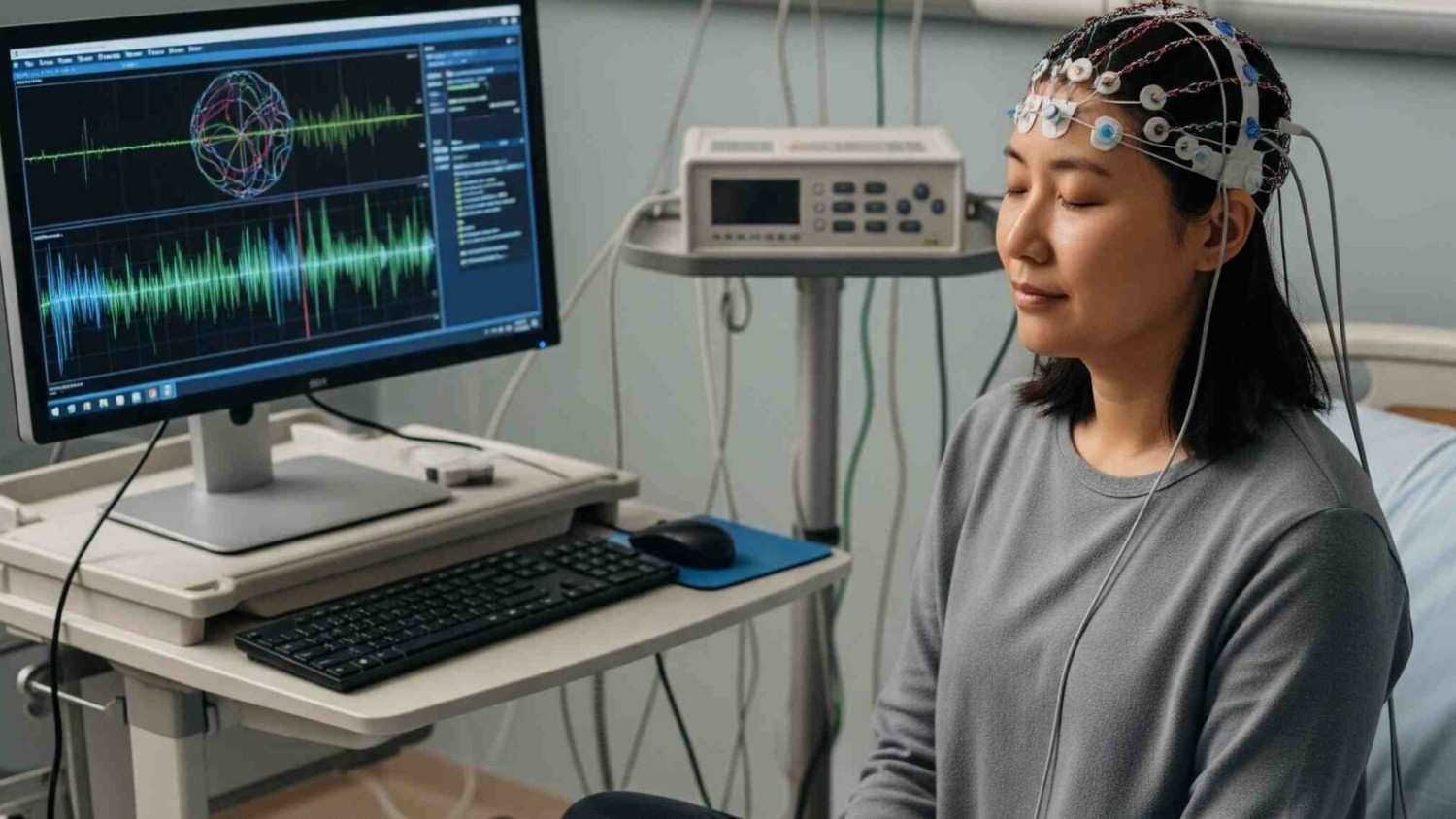
A typical session of Neurofeedback starts with placing small sensors, mostly EEG, on your scalp to track brain activity. You sit comfortably and watch or hear movies, images, and sounds, or even game plays.
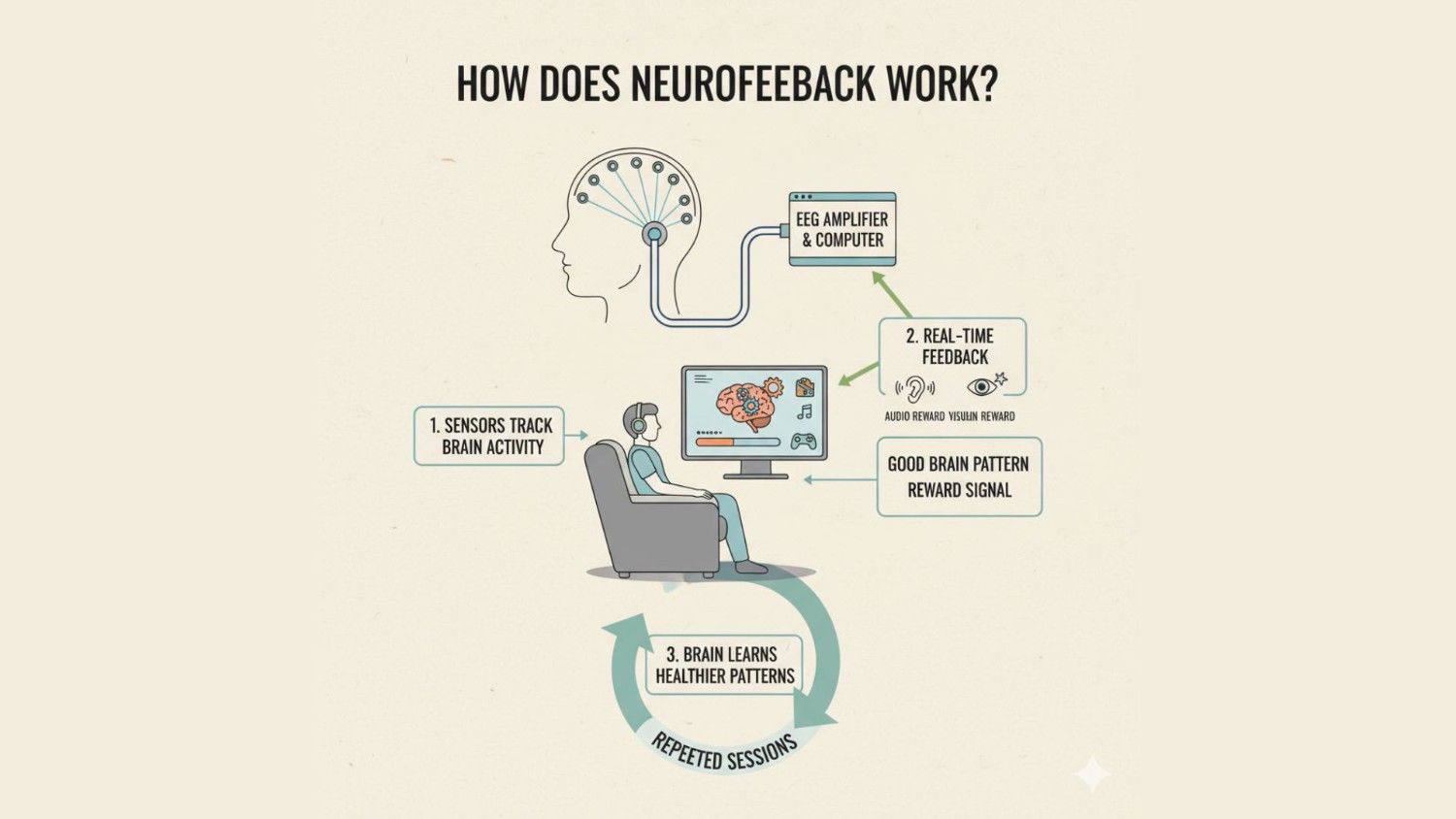
When the session is running, you receive instant feedback, so when your brain is following a good pattern, like making more alpha waves, you receive a reward signal either as audio or visual.
When this system is repeated over and over, your brain learns to repeat the healthier patterns on its own.
1. Understanding Brain Waves
The brain produces electrical oscillations called brain waves. Each frequency is linked to specific mental states:
- Delta (<4 Hz): deep sleep and recovery.
- Theta (4–8 Hz): drowsiness, memory processing, and sometimes inattention.
- Alpha (8–13 Hz): relaxed alertness and calm focus.
- Beta (13–30 Hz): active thinking, attention, and problem solving.
- Gamma (>30–80 Hz): high-level processing and integrating information.
When these rhythms become imbalanced, mental health symptoms can appear.
For example, too many theta waves are often seen in ADHD, while low alpha is linked with anxiety. A comprehensive tutorial by Enriquez-Geppert et al. (2017) highlights these brain wave–state relationships

Research shows neurofeedback can normalize these rhythms. Nicholson et al. (2023) found restored alpha activity in PTSD patients’ default mode network, alongside reduced symptoms after training
2. Areas Of The Brain Transformed
There are many regions that the human brain is divided into. These are the ones that Neurofeedback affects based on the condition:
1. Prefrontal cortex (front of the brain): This area controls attention, planning, and impulse regulation. Many ADHD protocols train prefrontal activity.
In a double-blind study, Bach-Morrow et al. (2022) showed that children who increased 14–18 Hz activity in the prefrontal cortex also improved executive functions compared to a placebo

2. Sensory-motor cortex (middle/top of brain): Neurofeedback often uses SMR training (12-15 Hz), which reduces hyperactivity and improves coordination.
For example, a study in healthy adults showed SMR up-training relieved anxiety and increased connectivity between sensorimotor regions.

3. Limbic system (deep inside the brain, includes the amygdala and hippocampus): This region handles emotions and stress.
A simultaneous fMRI-EEG study by Dehghani et al. (2023) showed that neurofeedback increased connectivity between the limbic system and prefrontal areas, improving emotional regulation
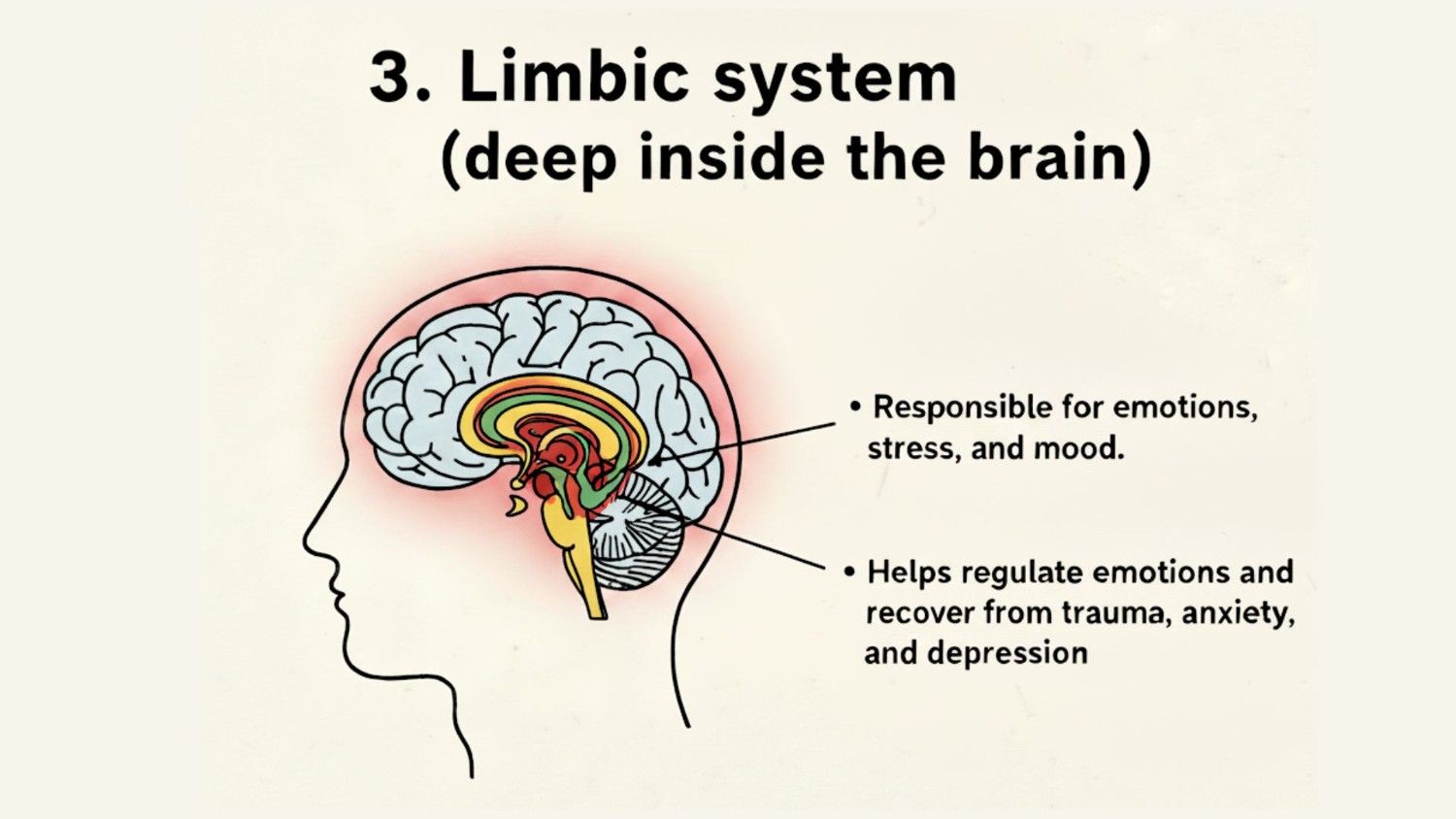
Another proof-of-concept trial in depression (Zotev et al., 2019) found that participants could upregulate amygdala activity and improve mood using combined EEG-fMRI feedback
3. Neurofeedback Changes In Brain Activity
Over multiple sessions, neurofeedback leads to measurable neural changes:
- Wave modulation: Harmful patterns like excess theta reduce, while alpha or beta activity stabilizes.
- Synaptic reinforcement: Brain networks supporting these healthy rhythms strengthen over time.
- Connectivity shifts: Regions such as the prefrontal cortex, parietal lobes, and limbic system show improved coordination.
These effects are not just short-term. A meta-analysis by Deilami et al. (2016) found that neurofeedback significantly reduced ADHD symptoms, with improvements comparable to stimulant medication.
Similarly, Rubia et al. (2019) reported that adolescents with ADHD who underwent fMRI neurofeedback showed lasting improvements in fronto-striatal connectivity, a network critical for self-control.
Together, these findings suggest that Neurofeedback does more than provide temporary relief, and it can rewire brain function in ways that support long-term recovery.
Conditions Treated With Neurofeedback
Neurofeedback can produce both short and long-term changes, with some conditions like ADHD improving relatively quickly, while others like autism or mood regulation may take consistent training.
Here’s a closer look at the conditions it can support:
- ADHD (children, teens, adults): Neurofeedback can improve attention, focus, and self-regulation. Studies show reductions in impulsivity and hyperactivity, with effects often lasting beyond the training sessions.
- Autism Spectrum Disorders: Emerging evidence suggests neurofeedback may help with attention, emotional regulation, and social responsiveness in some individuals on the spectrum.
- Anxiety and Depression: Neurofeedback can reduce symptoms of anxiety and help regulate mood in depression. Research shows improvements in emotional self-regulation and stress management after consistent sessions.
- Sleep and Insomnia: Training can improve sleep quality by helping the brain maintain more balanced activity patterns, supporting better rest and recovery.
- Memory, Learning, and Cognitive Performance: Neurofeedback has been linked to enhancements in working memory, focus, and academic performance, especially in children and young adults.
- Migraines: Some studies suggest neurofeedback may reduce migraine frequency and intensity by regulating cortical excitability.
Overall, Neurofeedback therapy seems to work best when the brain is running either too fast, as in anxiety or insomnia, or too slow, as in inattention and fatigue.
For further reading and evidence, refer to our references page.
Overarousal vs Underarousal Patterns
Our brains can be too “on” or too “off” in certain states. This is how Neurofeedback is helpful here:
1. Overarousal: You feel anxious, hyper, restless, and find it hard to sleep. Brain waves like high beta or many fast waves may dominate. Neurofeedback helps calm the brain, reduce excessive activity, and increase slower stabilizing waves.

2. Underarousal: You feel sluggish, tired, have trouble focusing, and feel mentally foggy. Some waves, like theta, may dominate when you need alertness. Neurofeedback can boost faster waves (beta, gamma) in relevant brain regions to increase focus.

Neurofeedback aims to move from extremes toward balance. The exact protocol depends on which side of the brain your brain tends toward, what your symptoms are, and where in the brain the problem occurs.
Types Of Neurofeedback Therapy
There are many different forms of Neurofeedback therapy, and the option depends on your conditions and available resources.
1. Frequency / Power Neurofeedback
This is the most common type. It uses 2-4 electrodes placed on the scalp to monitor specific wave frequencies.
Based on what you need, you get real-time feedback when the brain moves toward the desired frequency power. It has the largest body of research, especially for ADHD, anxiety, and insomnia.
2. Slow Cortical Potential Neurofeedback (SCP-NF)
SCP-NF trains your brain to change slow shifts in brain electrical voltage over seconds. These shifts reflect whether areas are more excitable or more inhibited.

It has shown efficacy in reducing ADHD symptoms and reducing seizures for epilepsy, with trials (using SCP protocol) demonstrating medium-to-large improvements.
It requires many sessions to learn to control these potentials effectively.
3. Low-Energy Neurofeedback System (LENS)
LENS uses very weak electromagnetic pulses rather than letting you consciously shift brain waves. The patient sits quietly, often with eyes closed.
The system delivers small signals to gently shift brainwave patterns automatically. It has been tried for traumatic brain injury, ADHD, insomnia, fibromyalgia, and mood problems. Evidence is more preliminary.
4. Hemoencephalographic (HEG) Neurofeedback
HEG monitors blood flow in parts of the brain, typically the cortex, rather than electrical waves. The feedback tells whether the blood flow is increasing or decreasing.

You learn to increase blood flow in targeted brain areas. It has been used in migraine treatment and has shown promise for improving attention.
5. Live Z-score Neurofeedback
In live Z-score neurofeedback, your brain activity is compared continuously to a normal database (people of the same age, etc.).

Differences from “normal” patterns are tracked, and you get feedback to correct them (for instance, LORETA-oriented live Z-score studies in depression show correction of dysfunctional source activity).
Many use this for insomnia, and sometimes for more complex patterns in ADHD or mood disorders.
6. Low-Resolution Electromagnetic Tomography (LORETA)
LORETA uses many EEG electrodes (often 19) and computational methods to estimate where, in 3D, inside the brain, the electrical activity comes from.
This lets feedback target deeper brain structures or networks. Applications include mood disorders, addiction, traumatic brain injury, and OCD.
Evidence includes eLORETA-based neurofeedback in depression showing changes in current source densities in prefrontal regions associated with symptom change.
LORETA does not directly measure deep sources, but provides mathematical estimates based on scalp EEG.
7. Functional Magnetic Resonance Imaging (fMRI) Neurofeedback
fMRI neurofeedback uses MRI machines in real time to show brain activity (blood flow changes) inside brain regions. You try to regulate the activity of parts seen in the MRI.

fMRI has been used for depression, emotion regulation, and PTSD. It offers good spatial detail but is expensive, slower (blood signals lag), and less accessible.
Benefits & Effectiveness Of Neurofeedback Therapy
Neurofeedback is non-invasive and drug-free. Meta-analyses show it yields lasting reductions in ADHD symptoms at 6-12-month follow-ups after 20-40 sessions, and produces large symptom drops in PTSD trials.
Research is ongoing, but these are the emerging benefits:
- Non-invasive and drug-free, reducing reliance on medication.
- Early sessions often improve sleep, focus, and reduce anxiety in some trials.
- Lasting benefits are more likely with longer programs of 30–40 sessions and follow-ups.
- ADHD trials show reduced symptoms after 20–30 sessions.
- Outcomes vary depending on the severity of the condition, consistency, and protocol design.
- Effectiveness can improve when combined with other therapies.
While results differ for each person, studies indicate that Neurofeedback can offer both short-term improvements and longer-term changes, making it a promising area for ongoing treatment research.
Limitations Of Neurofeedback Therapy
Neurofeedback takes time and effort, with most studies showing benefits only after many repeated training sessions.
Here are some limitations of neurofeedback therapy:
- Early improvements can fade without practice or follow-up care
- Some participants never learn to control the feedback signal
- Evidence is uneven due to small studies and weak control
- Outcomes vary depending on equipment, protocol, and clinician skill
Results are often modest for some conditions, and effectiveness depends strongly on how the therapy is delivered.
What To Expect During A Neurofeedback Therapy Session?
At first, you’ll do an assessment that often involves brain mapping or quantitative EEG (qEEG) to see what your brain waves look like in different states, so the clinician can know which frequencies or locations are off balance.

Then, during sessions, you wear sensors or electrodes and sit in a comfortable chair, often watching a screen or listening to tones.
Feedback comes in real-time. When your brain is doing “better,” you might see a game move, a bar rise, or hear a soothing sound. Or when it strays, you’ll get a cue to adjust. It’s non-invasive with no surgery or drugs during the session.
Programs usually require 20-40 sessions. Typically, two to three sessions are held each week, and the duration depends on the severity.
For mild issues, a lower-end approach may be sufficient, but for more serious or long-standing issues, additional sessions will be required. Each session often lasts 30-60 minutes, depending on the protocol and setup.
Risks & Considerations Of Neurofeedback Therapy
Sometimes, after sessions, people report mild side effects, like fatigue, a mild headache, and irritability, which tend to pass quickly.
Rare cases of overstimulation can happen if the protocol pushes the brain too far. Neurofeedback involves electrical or blood flow monitoring; the quality of the equipment matters.
It should be done under the supervision of a trained professional to avoid misuse. Also, cost and time commitment are significant.
Who Should Avoid Neurofeedback Therapy?
People with certain health conditions should be cautious with Neurofeedback. Take note for:
- Protocols need to be carefully designed for patients with epilepsy to avoid overstimulation.
- Patients who cannot or will not commit to multiple sessions (20-40, regular frequency) may get little or no benefit.
- People with severe psychiatric disorders where medical supervision is needed should only undertake under specialist care.
The bottom line is that you should always consult a licensed healthcare professional before starting any treatment.
Neurofeedback Therapy Cost & Accessibility
The cost of neurofeedback varies depending on your location, the level of protocol advancement, and who is administering it. Clinics sometimes offer package deals of around 20-40 sessions, which reduces the cost per session.
In India, a single session can range from Rs. 2,000 to Rs. 10,000, and some package deals can go up to Rs. 60,000 to Rs. 3,00,000 for a 30-day programme.
Accessibility depends heavily on local clinics with trained personnel. In many places, neurofeedback centers are rare. Advanced forms (such as LORETA and fMRI) are typically used in research or specialized clinics.
Sometimes equipment for home neurofeedback is available, but quality and supervision are crucial, and unsupervised/self-guided versions typically have weaker evidence.
Does Insurance Cover Neurofeedback Therapy?
Most insurers do not cover neurofeedback or only cover partial costs.
Some insurance plans may reimburse when used for epilepsy or ADHD in certain cases, but often only if prescribed by approved clinicians.
Part of the problem is that protocols vary greatly, and many insurers require strong clinical trials or standardization before agreeing to cover.
If you are considering neurofeedback, check with your insurance provider in advance. Ask whether the provider is approved, whether the condition qualifies, and whether the specific protocol is accepted.
Tips To Choose The Right Neurofeedback Provider
Choosing a Neurofeedback centre or clinic that fits your needs could be confusing if you are new to the options. Keep these points in mind when choosing a Neurofeedback provider to avoid confusion –
1. Certification & training: Look for professionals certified by bodies such as the BCIA (Biofeedback Certification International Alliance) or similar. They should have training in neurofeedback, EEG, qEEG, and safety protocols.
2. Protocol & equipment: Ask what technique they plan to use (frequency/power, SCP, LORETA, etc.), what kind of sensors/electrodes and software, and whether assessment (qEEG) is used to tailor therapy. Advanced equipment is good only if they know how to use it.
3. Track record & case histories: Look for before/after data, follow-up results. Patient reviews and published outcome data are helpful.
4. Trial session or assessment: Good providers often begin with an evaluation or trial to see whether you respond, and adjust protocol accordingly.
5. Support & integration: See if neurofeedback will be combined with other therapies like behavioral therapy and lifestyle changes. Neurofeedback alone might not be the most effective for severe cases.
During any medical procedure, including neurofeedback, safety, comfort, and assurance are the most important. Hence, it is best to take your own time and make a decision.
Conclusion: Neurofeedback Therapy Is A Non-Invasive Treatment For Many Psychological Conditions
Neurofeedback therapy offers a non-invasive, drug-free way to help the brain change its activity toward healthier patterns. It has shown real promise in treating ADHD, epilepsy, PTSD, and other conditions.
Many studies report improvements, especially when treatment is prolonged and administered by trained professionals.
But it is not magic. Effects vary by person, protocol, and condition. The Neurofeedback therapy demands commitment because it requires time, cost, and consistency.
If you are considering neurofeedback, a good starting point is Brain&Co’s free 2-minute brain assessment available on the WeTrainBrains website.
You can also book a free consultation with our specialists to discuss your results and explore whether neurofeedback is the right approach for you.
FAQs
Small clinical trials in student populations suggest neurofeedback may reduce moderate anxiety.
Most protocols use 2-3 sessions per week. Consistency matters. Frequent sessions help the brain learn faster and maintain change.
Many clinicians combine neurofeedback with therapy (talk therapy, CBT), medication, and lifestyle changes for better results. Neurofeedback often supports or enhances other treatments.
Some gains can drop off if you stop altogether, especially early in treatment. But many studies indicate that when the protocol matches the condition and sessions are sufficient, improvements persist for months. Booster sessions or maintenance may help.
The procedure is non-invasive. You wear sensors or electrodes on your scalp. Some people report mild discomfort from the equipment, as well as mild headaches or fatigue, which typically recover quickly; however, physical pain is very rare.





